- RAG rating
- n/a
- Document type
- Clinical policy
- Place
- Hertfordshire and West Essex ICB
- Output type
- Clinical Policies & Evidence-based Interventions
- Document
- Download
Epidural Injections and Therapeutic Nerve Blocks for Lumbar or Sacral Radiculopathy
July 2022 v1.0
This policy covers epidural injections and therapeutic nerve root blocks for lumbar or sacral radiculopathy. Other sites, e.g., cervical or thoracic are outside the scope of this policy. Interventions for non-specific back pain are outside the scope of this policy and are covered in the local policy:
Injections and radio-frequency ablation for non-specific back pain.
Link to website: Evidence Based Intervention Policies – Hertfordshire and West Essex NHS ICB
- Injections for non-specific back pain without sciatica – EBI list 1
- Lumbar radiofrequency facet joint denervation – EBI list 2
- Low back pain imaging – EBI list 2
- Lumbar discectomy – EBI list 2
- Vertebral augmentation for painful osteoporotic vertebral fractures – EBI list 2
- Fusion surgery for mechanical axial low back pain – EBI list 2
Other related local policies:
- Spinal cord stimulation. Link to website Evidence Based Intervention Policies – Hertfordshire and West Essex NHS ICB
- Injections and radio-frequency ablation for non-specific back pain. Link to website Evidence Based Intervention Policies – Hertfordshire and West Essex NHS ICB
Epidural Injections and Therapeutic Nerve Root Blocks
The ICB will fund epidural injections of local anaesthetic and steroid, providing all of the criteria below have been met: 1,3,4
- The patient is 16 years or older. 4
AND
- The patient has radicular pain consistent with the level of spinal involvement.
AND
- The pain is having a significant impact upon the patient’s ADLs (this will need to be clearly documented)
AND
- The pain has persisted despite non-invasive management as per local pathways and the national back pain pathway (advice on self-management, analgesia, exercise programme +/- manual therapy +/- psychological therapy OR low intensity CPPP) UNLESS an MDT agrees that there is acute severe radiculopathy in which case this criterion may be waived.
AND
- Patients must have actively participated in the decisions in respect of their treatment and demonstrated commitment to their long-term treatment plan.
AND
- The pain is due to prolapsed intervertebral disk.
AND
- The pain is acute (<3 months) at the time of referral.
AND
- The pain is severe and uncontrollable (rated at 7/10 or more on the visual analogue pain scale).
OR
- The pain is due to inflammatory or compressive causes.
AND
- The pain is moderate (5/10 or more on visual analogue pain scale) or severe.
AND
- The pain having lasted more than 6 months.
AND
- The aim is to avoid surgery (reflecting patient and clinician choice) or surgery is contraindicated or not feasible.
The ICB will not routinely fund epidural injections for patients with non-specific low back pain1 or for neurogenic claudication in people who have central canal stenosis. 1,3,4
Repeat Epidural/Therapeutic Nerve Block.
The ICB will not routinely fund repeat epidural or therapeutic nerve block injections for acute and severe lumbar radiculopathy due to prolapsed intervertebral disk.
The ICB will fund repeat epidural or therapeutic nerve block injections for moderate to severe chronic radicular pain due to inflammatory or compressive causes when the following criteria are met:
- 6 months of benefit and functional improvement was achieved following the previous injection.
- Patients must show commitment to taking responsibility for managing their condition by demonstrating relevant lifestyle changes which include weight loss, increased physical fitness through exercise and physiotherapy; diet control, avoidance of illicit drugs and alcohol, improvement in sleep hygiene, engaging with activities to promote mental wellbeing and any treatment plans for mental health problems, and improved engagement in activities of daily living and purposeful occupation where appropriate or not able to participate in such activities.
Rationale
NICE NG59 does not address repeat epidurals in the summary guidance. However, in the full guidance, it describes that there is only evidence for the acute (<3month) presentation and that the guideline development group did not expect multiple injections to be performed within the short period of time defined as acute. The available cost effectiveness evidence suggests that repeats are not cost effective.
Initial cost-effectiveness data suggests a cost of £45K per QALY (not cost effective). This was based on 1-3 injections over 6 months compared with placebo. A sensitivity analysis was performed which assumed a single injection (based on the expectation that only one injection would be performed within the short period of time defined as acute) but assumed the same health benefits as 1-3 injections. This changed the cost effectiveness estimate to £26k per QALY (cost effective) which led to NICE supporting epidural injections in acute and severe radiculopathy.
However, NICE excludes patients with conditions of a non-mechanical nature, including inflammatory causes and serious spinal pathology (including osteoporotic collapse), also spondylisthesis, scoliosis, vertebral fracture, OA, FBSS etc.
The GIRFT states that epidurals/nerve root injections may be done in the hope radicular pain due to foraminal or lateral recess stenosis or disc protrusion settles. If it does not provide prolonged pain relief, then surgery is often an alternative option with a sound evidence base, including cost-effectiveness. There should therefore be few patients needing 3 or more epidurals/nerve root injections in a 12-month period. The GIRFT report recommendation is that clinicians should adhere to the National Back Pain and Radicular Pain Pathway, which has been endorsed by NICE.
The National Back and Radicular Pain Pathway says that injection of depot preparations of steroid, usually with local anaesthetic, has an established value in a variety of acute and chronic pain problems associated with inflammatory, compressive or post-surgical pathology in lumbrosacral spine, where leg pain is predominant symptom. However, it is unclear what evidence this is based on as this is not addressed within any of the referenced literature.
The National Back and Radicular Pain Pathway suggests the following indications for epidurals/nerve root injections:
- Severe, non-controllable radicular pain in prolapsed intervertebral disc, early in clinical course (i.e., acute)- Moderate or severe lumbrosacral radicular pain (compressive or inflammatory) with aim of avoiding surgery (patient and clinician choice)- Lack of suitability of alternative treatments (e.g., unfit for surgery, poorly defined surgical target, unable to tolerate neuropathic pain medications – especially elderly)
o Combine with appropriate medication management, physical and psychological therapies to maximise benefit.
Appendix 1
The Back Pain Pathway Flowchart
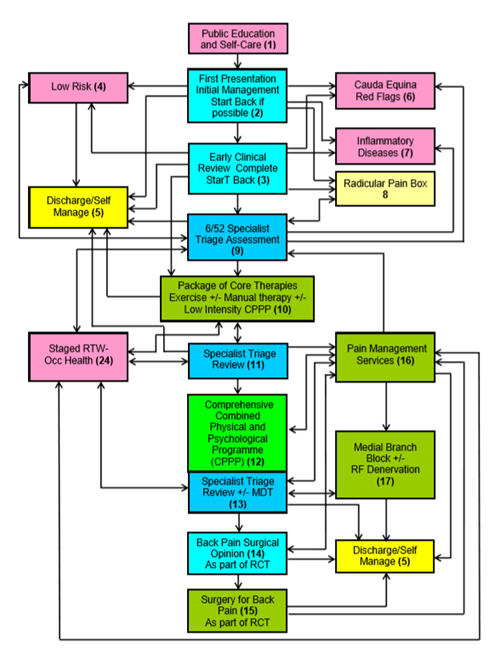
Source: extracted from the National Low Back and Radicular Pain Pathway 2017, page 14(3).
The Radicular Pain Pathway Flowchart
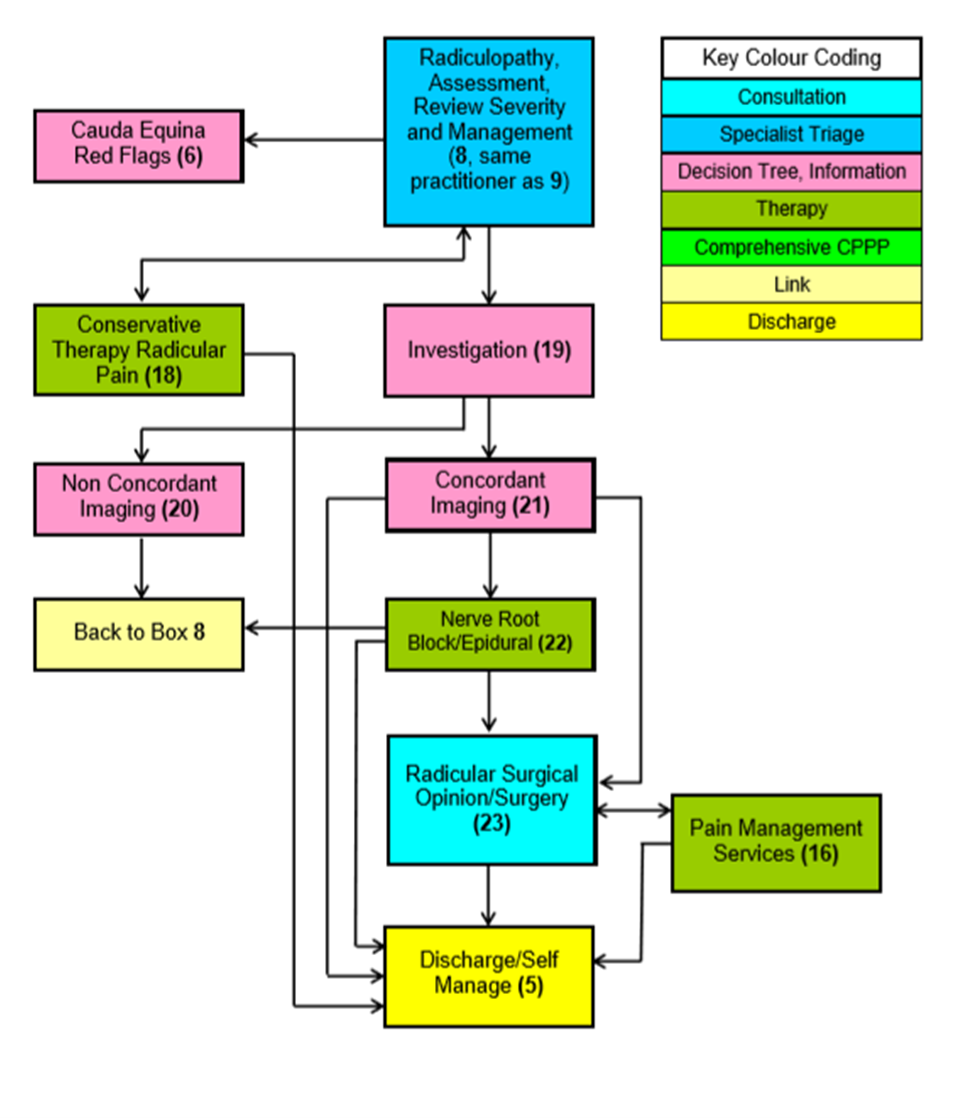
Source: extracted from the National Low Back and Radicular Pain Pathway 2017, page 15(3)
Appendix 2: Non-invasive management
A list of non-invasive treatments for low back pain and sciatica approved by NICE and recommended by the National Low Back and Radicular Pain Pathway.
NICE approves the following non-invasive treatments for low back pain and sciatica(4):
- Guided self-management.
- Exercise (ideally group programme)
- Manual therapy (spinal manipulation, mobilisation, or soft tissue techniques such as massage) for managing low back pain with or without sciatica, but only as part of a treatment package including exercise, with or without psychological therapy.
- Psychological therapies using a cognitive behavioural approach for managing low back pain with or without sciatica but only as part of a treatment package including exercise, with or without manual therapy (spinal manipulation, mobilisation or soft tissue techniques such as massage).
- Consider a combined physical and psychological programme, incorporating a cognitive behavioural approach (preferably in a group context that takes into account a person's specific needs and capabilities), for people with persistent low back pain or sciatica:
- when they have significant psychosocial obstacles to recovery (for example, avoiding normal activities based on inappropriate beliefs about their condition) or- when previous treatments have not been effective
- Return-to-work programmes (promote and facilitate return to work or normal activities of daily living).
- Pharmacological interventions
The National Back Pain Pathway also recommends(3):
- Public Education and self-care
- GP or over the counter medication
- Self-directed exercise programme
- Self-directed relaxation techniques
- Self-directed return to normal social and occupational activities
- Core therapies: Exercise o +/- Manual therapy o +/- Low intensity CPP (as appropriate)
- Comprehensive multi-disciplinary M-CPPP or Pain Management Programme
Appendix 3
Back pain injections are commonly defined in terms of the anatomical structures targeted and whether the drug injected is being used for therapeutic or diagnostic effect.
The types of injections are:
- Therapeutic facet joint injections including: intra-articular facet joint injection, medial branch block injection
- Therapeutic epidural injections including (according to where the epidural space is accessed) which could be lumbar epidural or caudal epidural injections.
- Diagnostic which helps in to determine the anatomic origin of the patient’s pain.
Clinical features suggestive of a facet joint component 3
- "Increased pain unilaterally or bilaterally on lumbar para-spinal palpation
- Increased back pain on 1 or more of the following:
- Extension (more than flexion)
- Rotation
- Extension/side flexion
- Extension/rotation
AND
- No radicular symptoms
- No sacroiliac joint pain elicited using a provocation test.”
Epidural injection
Steroid medication can also be given as an epidural injection to treat back, or leg pain caused by sciatica or a slipped (prolapsed) disc.
The epidural can be inserted at different levels of your back depending on the area of the body that requires pain relief.
There are different types of epidural depending on the approach taken: caudal, interlaminar and transforaminal.”
Facet joint" The spine is a column of bones arranged one on top of the other. The bones are linked at the back by joints called facet joints, on each side. The facet stabilises the spine, while also allowing movement”
Facet joint injection
"Under x-ray control, local anaesthetic (to reduce pain in the short-term) and corticosteroid (to reduce pain and inflammation in the long-term) are injected into the targeted facet joints.”
Lower back pain
Non-specific back pain
Most people's back pain is described as non-specific, meaning it’s caused by a minor problem with the structures in the back (such as a strain) rather than anything serious.
The back is a complex area of muscles, nerves, bones and joints, and is continuously working hard to support the weight of the upper body.
It’s often unclear why lower back pain occurs, but it can sometimes be triggered by things like bending awkwardly, lifting incorrectly, standing for long periods of time, slouching when sitting, and driving for long periods. Sometimes lower back pain will come and go over time
Medial branch blocks(6)
"Facet joint medial branch blocks is a procedure in which nerve fibres supplying the painful facet joints are blocked by local anaesthetic injections.”
Radiofrequency denervation(9)
"Radiofrequency denervation is a specialised injection, which uses heat to alter the function of the nerves that supply the facet joints in your back. These nerves transmit the pain signals from these joints to your brain. The procedure carried out using X rays to guide the injections, in a similar way to diagnostic tests.
Radiofrequency denervation of the nerves is performed by placing special needles alongside the nerves to the facet joints, then passing an electric current through each needle. This creates heat at the needle tip, which results in a change to the structure and function of the nerve. This can lead to a reduction of pain.”
Sciatica or radiculopathy (7)
"Sciatica is pain caused by irritation or compression of the sciatic nerve. The sciatic nerve is the longest nerve in your body, and runs from the back of your pelvis, through your buttocks and down both legs, ending at your feet.
When something compresses or irritates the sciatic nerve, it can cause pain, numbness and a tingling sensation that travels from your lower back down your leg.
The most common cause of sciatica is a slipped (or prolapsed) disc. This occurs when one of the discs that sit between and cushion the bones in the spine is damaged and presses on nearby nerves. Most cases will pass in a few weeks or months, although it may come and go over time. Treatments such as staying active, painkillers, and back exercises or stretches often help. In rare cases, surgery may be needed.”
Spinal cord stimulation (neuromodulation)(10)
Steroid injections (11)
Steroids are a man-made version of hormones normally produced by the adrenal glands, two small glands found above the kidneys.
When injected into a joint or muscle, steroids reduce redness and swelling (inflammation) in the nearby area. This can help relieve pain and stiffness.”
References
- NHS England. Evidence-Based Interventions: Guidance for CCGs. (2.0):180.
- Hutton M. Spinal Services GIRFT Programme National Specialty Report [Internet]. 2019. Available from: https://gettingitrightfirsttime.co.uk/wp-content/uploads/2019/01/spinal-surgery-report.pdf
- NHS England. National Low Back and Radicular Pain Pathway 2017. 2017.
- National Institute of Healthcare and Clinical Excellence. Low back pain and sciatica in over 16s: assessment and management Invasive treatments NICE Guideline NG59 [Internet]. 2016. Available from: https://www.nice.org.uk/guidance/ng59
- NHS. Overview: Epidurals [Internet]. 2017 [cited 2006 Sep 20]. Available from: https://www.nhs.uk/conditions/epidural/
- Guy’s and St Thomas’ NHS Foundation Trust. Facet joint medial branch blocks for the treatment of pain. 2017.
- NHS. Overview: Back Pain [Internet]. 2017. Available from: https://www.nhs.uk/conditions/back-pain/
- Oxford University NHS Trust. Radiofrequency Denervation of the lumbar facet joints- Information for patients. 2015.
- 1NHS. Steroid injections [Internet]. 2017 [cited 2006 Sep 20]. Available from: https://www.nhs.uk/conditions/steroid-injections/